So…You Want to be an SVC Pro: Is “More Chemo” Your Final Answer?
- sbord1
- Nov 2, 2021
- 5 min read

CASE
A 53-year-old male presents with multiple episodes of provoked and unprovoked syncope in the last 3 days, with associated shortness of breath and right-sided facial, ear and neck swelling. The patient reports that over-the-counter antihistamine treatment has mildly relieved some of the swelling, but the shortness of breath intermittently worsens with exertion.
- Past Medical History:
o Stage IIIC (T4N3M0) squamous cell carcinoma of the lung in the right upper lobe s/p chemo and radiation (diagnosed, treated three years ago), radiation pneumonitis
- Recent RUE DVT in the last 3 weeks (confirmed on Doppler ultrasound at last ED visit, started on DOAC)
Figure 1. Coronal chest CT with right lung mass; white arrow: azygos vein dilation(1)
- Patient endorses remote smoking history and intermittent uneasiness, but denies any confusion, changes in vision, urinary incontinence, oral trauma, and has no personal or family history of cardiac or cerebrovascular disease. The remainder of ROS was negative. His only remarkable exam finding was decreased sensation in the right posterior auricular dermatome with mild unilateral submandibular edema.
Clinical question: What is superior vena cava syndrome, and how can providers recognize and manage its various presentations in the ED?
SUMMARY OF EVIDENCE
- Superior vena cava (SVC) syndrome describes the clinical effects secondary to mechanical obstruction of the SVC2. Obstruction of SVC can occur either directly or indirectly (via brachiocephalic trunk or subclavian vein compression), and can originate from the intravascular (e.g. thrombosis) or extravascular space (e.g. malignancy)(1).
- More than two-thirds of SVC syndrome cases are secondary to malignant masses (e.g. lung cancer, breast cancer, lymphoma), and the remaining third are caused by benign masses (e.g. thymomas, cystic hygromas, thyroid goiter) or intravascular pathology (e.g. thrombosis from vascular catheters, pacemaker leads, aortic aneurysms)(1-3).
- Thrombosis is also a long-term sequela of SVC syndrome and is most commonly found in deep vasculature of the upper extremities (subclavian, axillary or brachiocephalic veins)(4).
Symptoms
- The most typical clinical presentation includes dyspnea and facial fullness or swelling. Additional common symptoms are cough, chest pain and dysphagia3. In the most severe scenarios of SVC compression (with impaired collateral venous flow through the inferior vena cava (IVC) and azygos veins), plethora, acute laryngeal edema and cerebral herniation can result (3, 5-6).
- While an unstable airway can result during the most unusually acute presentations, mechanical ventilation is rarely indicated in the ED. Any resulting laryngeal edema is most likely to cause obstruction in the upper airway, which would necessitate the use of transtracheal jet ventilation or cricothyroidotomy (in the most critical scenarios), not endotracheal intubation2. Additionally, stenting is known to provide superior, more rapid relief of symptoms and decreased recurrence of SVC syndrome in patients with known tumors, compared to chemotherapy and/or radiation(2).
- A recent classification system (Table 1) developed by Yu et. al stratifies risk based on presenting symptoms(5). Insights from this proposed system enables ED providers to better triage patients who may require more urgent management.
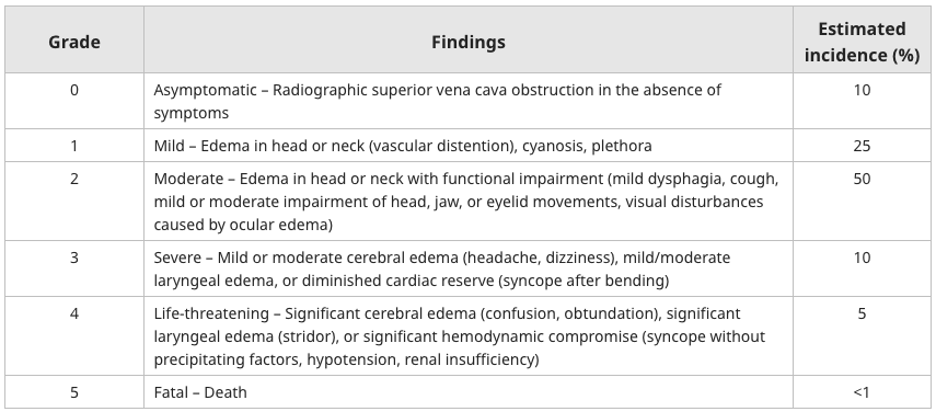
Table 1. Proposed classification system for malignant superior vena cava syndrome(5*)
MANAGEMENT:
- While diagnosis of SVC is clinical, imaging (CT/MRI with contrast) confirms the diagnosis6. Imaging can provide additional information about etiology, which can guide downstream management (e.g. new/recurrent malignancy, deep vein thrombosis progressing to pulmonary embolism).
- Typical management varies based on grade(6):
o Patients with symptoms classified as Grade 1 or 2 can receive an elective CT. If thrombosis is found on imaging, anticoagulation is mainstay treatment. If tumor is found on imaging, arrange for biopsy to stage, treat or refer to palliative care.
o Patients with Grade 3 or 4 symptoms should receive urgent and emergent CT, respectively. If thrombosis is noted on imaging, treat with thrombolysis (unless secondary to known malignancy, such as patient in case study). If tumor is seen on imaging, intravascular stenting is accepted as superior treatment for patients in acute settings compared to chemotherapy and/or radiation.(7-9)
- Additional studies are needed to determine efficacy of ancillary treatments
o There is no evidence that raising the head of the bed reduces intracranial or intrathoracic pressure(10). There is limited evidence that oxygen administration, diuretics and steroids improve symptoms (6).
o Based on the Kishi scoring system (Table 2), intervention should be considered for a score of 4 or greater (6).
Signs and Symptoms Score
Neurologic Symptoms
Stupor, coma, or blackout 4
Blurry vision, headache, dizziness, or amnesia 3
Changes in mentation 2
Uneasiness 1
Laryngopharyngeal or thoracic symptoms
Orthopnea or laryngeal edema 3
Stridor, hoarseness, dysphagia, 2
glossal edema, or shortness of breath
Cough or pleural effusion 1
Nasal and facial signs or symptoms
Lip edema, nasal stiffness, epistaxis, or rhinorrhea 1
Facial swelling 1
Venous dilation
Neck vein or arm vein distension, 1
upper extremity swelling, or upper body plethora
RECOMMENDATIONS:
1. Obtain imaging early in clinical course for patients with signs and symptoms consistent with SVC syndrome to appropriately grade and direct appropriate management
2. Treatment plan for imaging-confirmed thrombosis: Patients with Grade 1 or 2 symptoms should be discharged with anticoagulation medication. Patients with Grade 3 or 4 symptoms should be considered for anticoagulation or thrombolysis if hemodynamically unstable
3. Treatment plan for imaging-confirmed extravascular malignant compression: Patients with Grade 1 or 2 symptoms, stage with biopsy if unknown type, treat with chemotherapy and/or radiation therapy in outpatient setting otherwise. Patients with Grade 3 or 4 symptoms should be considered for intravascular stenting, as it decreases likelihood of recurrent SVC syndrome compared to chemotherapy and/or radiation.
REFERENCES
1. Cohen R, Mena D, Carbajal-Mendoza R, Matos N, Karki N. Superior vena cava syndrome: A medical emergency? Int J Angiol. 2008 Spring;17(1):43-6. doi: 10.1055/s-0031-1278280. PMID: 22477372; PMCID: PMC2728369.
2. Brock P, Cruz-Carreras MT. Emergency complications of malignancy. Tintinalli JE, Ma O, Yealy DM, Meckler GD, Stapczynski J, Cline DM, Thomas SH, editors. Tintinalli's Emergency Medicine: A Comprehensive Study Guide, 9e. McGraw Hill; 2020.
3. Long B. Oncologic Emergencies Part I: Pearls and pitfalls [Internet]. Koyfman A, Bright J, editors. emDOCs.net - Emergency Medicine Education. 2020 [cited 2021Oct10]. Available from: http://www.emdocs.net/oncologic-emergencies-part-i-pearls-and-pitfalls/
4. Joffe HV, Kucher N, Tapson VF, Goldhaber SZ; Deep Vein Thrombosis (DVT) FREE Steering Committee. Upper-extremity deep vein thrombosis: a prospective registry of 592 patients. Circulation. 2004 Sep 21;110(12):1605-11. doi: 10.1161/01.CIR.0000142289.94369.D7. Epub 2004 Sep 7. PMID: 15353493.
5. Yu JB, Wilson LD, Detterbeck FC. Superior vena cava syndrome--a proposed classification system and algorithm for management. J Thorac Oncol. 2008 Aug;3(8):811-4. doi: 10.1097/JTO.0b013e3181804791. PMID: 18670297.
6. Klein-Weigel PF, Elitok S, Ruttloff A, Reinhold S, Nielitz J, Steindl J, Hillner B, Rehmenklau-Bremer L, Wrase C, Fuchs H, Herold T, Beyer L. Superior vena cava syndrome. Vasa. 2020 Oct;49(6):437-448. doi: 10.1024/0301-1526/a000908. PMID: 33103626.
7. Aldoss O, Arain N, Menk J, Kochilas L, Gruenstein D. Endovascular stent provides more effective early relief of SVC obstruction compared to balloon angioplasty. Catheter Cardiovasc Interv. 2014 Jun 1;83(7):E272-6. doi: 10.1002/ccd.24413. Epub 2013 Dec 4. PMID: 22431347; PMCID: PMC4357311.
8. Sobrinho G, Aguiar P. Stent placement for the treatment of malignant superior vena cava syndrome - a single-center series of 56 patients. Arch Bronconeumol. 2014 Apr;50(4):135-40. English, Spanish. doi: 10.1016/j.arbres.2013.10.009. Epub 2013 Dec 18. PMID: 24360084.
9. Spring J, Munshi L. Oncologic emergencies: Traditional and contemporary [Internet]. Critical Care Clinics. Elsevier; 2020 [cited 2021Oct10]. Available from: https://www.sciencedirect.com/science/article/pii/S0749070420300579#fig2
10. Lepper PM, Ott SR, Hoppe H, Schumann C, Stammberger U, Bugalho A, et al. Superior vena cava syndrome in thoracic malignancies [Internet]. American Association for Respiratory Care. Respiratory Care; 2011 [cited 2021Oct10]. Available from: http://rc.rcjournal.com/content/56/5/653.full











Comments